Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells.
Protection
Blood has several roles in inflammation:
- Leukocytes, or white blood cells, destroy invading microorganisms and cancer cells
- Antibodies and other proteins destroy pathogenic substances
- Platelet factors initiate blood clotting and help minimise blood loss
Regulation
Blood helps regulate:
- pH by interacting with acids and bases
- Water balance by transferring water to and from tissues
Blood is classified as a connective tissue and consists of two main components:
- Plasma, which is a clear extracellular fluid
- Formed elements, which are made up of the blood cells and platelets
The formed elements are so named because they are enclosed in a plasma membrane and have a definite structure and shape. All formed elements are cells except for the platelets, which tiny fragments of bone marrow cells.
Formed elements are:
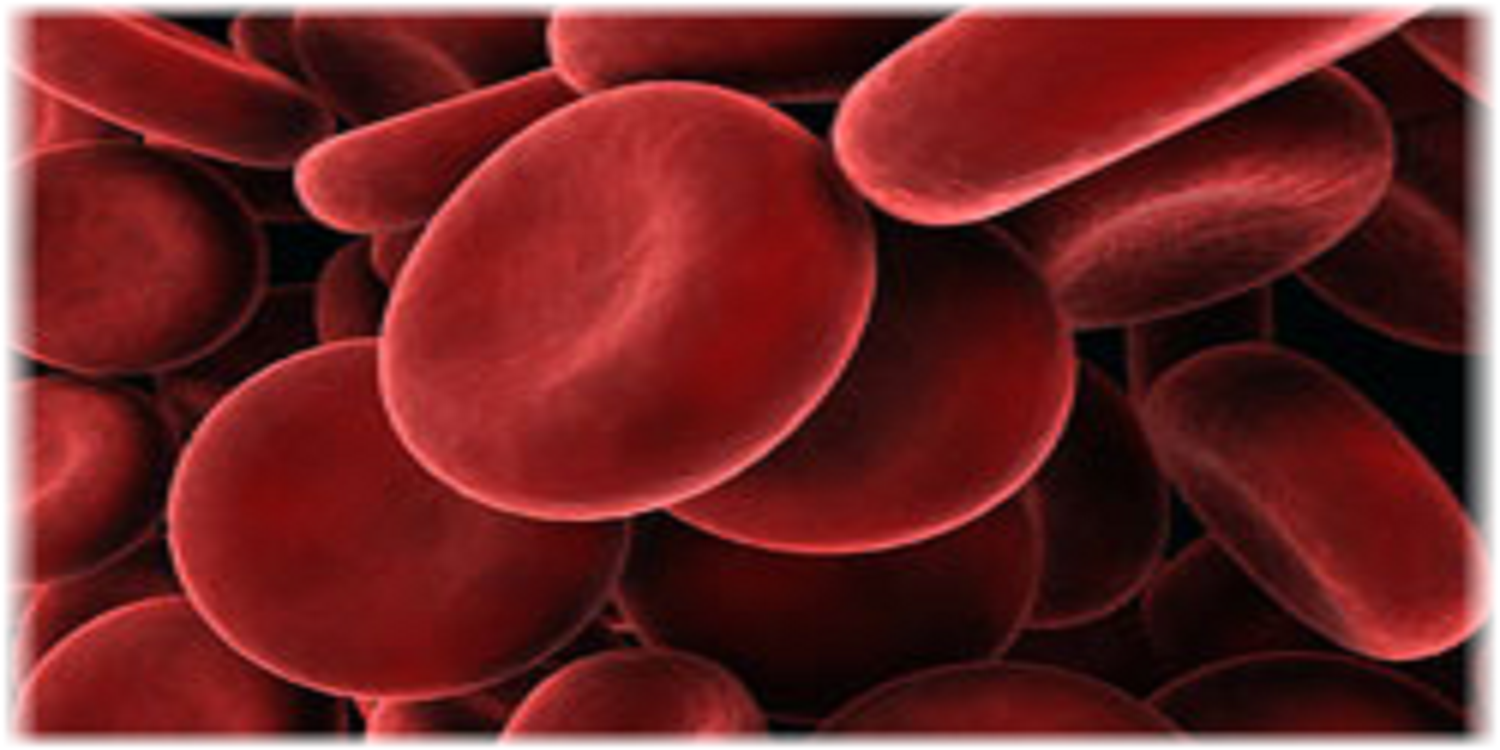
- Erythrocytes, also known as red blood cells (RBCs)
- Leukocytes, also known as white blood cells (WBCs)
- Platelets
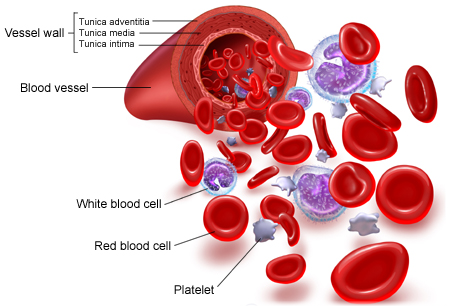 Leukocytes are further classified into two subcategories called granulocytes which consist of neutrophils, eosinophils and basophils; and agranulocytes which consist of lymphocytes and monocytes.
Leukocytes are further classified into two subcategories called granulocytes which consist of neutrophils, eosinophils and basophils; and agranulocytes which consist of lymphocytes and monocytes.
The formed elements can be separated from plasma by centrifuge, where a blood sample is spun for a few minutes in a tube to separate its components according to their densities. RBCs are denser than plasma, and so become packed into the bottom of the tube to make up 45% of total volume. This volume is known as the haematocrit. WBCs and platelets form a narrow cream-coloured coat known as the buffy coat immediately above the RBCs. Finally, the plasma makes up the top of the tube, which is a pale yellow colour and contains just under 55% of the total volume.
Blood plasma is a mixture of proteins, enzymes, nutrients, wastes, hormones and gases. The specific composition and function of its components are as follows:
These are the most abundant substance in plasma by weight and play a part in a variety of roles including clotting, defence and transport. Collectively, they serve several functions:
- They are an important reserve supply of amino acids for cell nutrition. Cells called macrophages in the liver, gut, spleen, lungs and lymphatic tissue can break down plasma proteins so as to release their amino acids. These amino acids are used by other cells to synthesise new products.
- Plasma proteins also serve as carriers for other molecules. Many types of small molecules bind to specific plasma proteins and are transported from the organs that absorb these proteins to other tissues for utilisation. The proteins also help to keep the blood slightly basic at a stable pH. They do this by functioning as weak bases themselves to bind excess H+ ions. By doing so, they remove excess H+ from the blood which keeps it slightly basic.
- The plasma proteins interact in specific ways to cause the blood to coagulate, which is part of the body’s response to injury to the blood vessels (also known as vascular injury), and helps protect against the loss of blood and invasion by foreign microorganisms and viruses.
- Plasma proteins govern the distribution of water between the blood and tissue fluid by producing what is known as a colloid osmotic pressure.
There are three major categories of plasma proteins, and each individual type of proteins has its own specific properties and functions in addition to their overall collective role:
- Albumins, which are the smallest and most abundant plasma proteins. Reductions in plasma albumin content can result in a loss of fluid from the blood and a gain of fluid in the interstitial space (space within the tissue), which may occur in nutritional, liver and kidney disease. Albumin also helps many substances dissolve in the plasma by binding to them, hence playing an important role in plasma transport of substances such as drugs, hormones and fatty acids.
- Globulins, which can be subdivided into three classes from smallest to largest in molecular weight into alpha, beta and gamma globulins. The globulins include high density lipoproteins (HDL), an alpha-1 globulin, and low density lipoproteins (LDL), a beta-1 globulin. HDL functions in lipid transport carrying fats to cells for use in energy metabolism, membrane reconstruction and hormone function. HDLs also appear to prevent cholesterol from invading and settling in the walls of arteries. LDL carries cholesterol and fats to tissues for use in manufacturing steroid hormones and building cell membranes, but it also favours the deposition of cholesterol in arterial walls and thus appears to play a role in disease of the blood vessels and heart. HDL and LDL therefore play important parts in the regulation of cholesterol and hence have a large impact on cardiovascular disease.
- Fibrinogen, which is a soluble precursor of a sticky protein called fibrin, which forms the framework of blood clot. Fibrin plays a key role in coagulation of blood, which is discussed later in this article under Platelets.
- Neutrophils: These contain very fine cytoplasmic granules that can be seen under a light microscope. Neutrophils are also called polymorphonuclear (PMN) because they have a variety of nuclear shapes. They play roles in the destruction of bacteria and the release of chemicals that kill or inhibit the growth of bacteria.
- Eosinophils: These have large granules and a prominent nucleus that is divided into two lobes. They function in the destruction of allergens and inflammatory chemicals, and release enzymes that disable parasites.
- Basophils: They have a pale nucleus that is usually hidden by granules. They secrete histamine which increases tissue blood flow via dilating the blood vessels, and also secrete heparin which is an anticoagulant that promotes mobility of other WBCs by preventing clotting.
This is a prompt constriction of the broken blood vessel and is the most immediate protection against blood loss. Injury stimulates pain receptors. Some of these receptors directly innervate nearby blood vessels and cause them to constrict. After a few minutes, other mechanisms take over. Injury to the smooth muscle of the blood vessel itself causes a longer-lasting vasoconstriction where platelets release a chemical vasoconstrictor called serotonin. This maintains vascular spasm long enough for the other haemostatic mechanisms to come into play.
Under normal conditions, platelets do not usually adhere to the wall of undamaged blood vessels, since the vessel lining tends to be smooth and coated with a platelet repellent. When a vessel is broken, platelets put out long spiny extensions to adhere to the vessel wall as well as to other platelets. These extensions then contract and draw the walls of the vessel together. The mass of platelets formed is known as a platelet plug, and can reduce or stop minor bleeding.
This is the last and most effective defence against bleeding. During bleeding, it is important for the blood to clot quickly to minimise blood loss, but it is equally important for blood not to clot in undamaged vessels. Coagulation is a very complex process aimed at clotting the blood at appropriate amounts. The objective of coagulation is to convert plasma protein fibrinogen into fibrin, which is a sticky protein that adheres to the walls of a vessel. Blood cells and platelets become stuck to fibrin, and the resulting mass helps to seal the break in the blood vessel. The forming of fibrin is what makes coagulation so complicated, as it involved numerous chemicals reactions and many coagulation factors.